How severe is your prolapse diagnosis? 
Are you worried you may need prolapse surgery?
Is your prolapse beyond repair without surgery? It‘s often confusing to understand your prolapse severity – especially if you’re feeling nervous and disappointed when receiving your diagnosis.
You can’t really see the full extent of your prolapse and it’s a little socially awkward to compare it to someone else’s.
The following Pelvic Floor Physiotherapist information is designed to help you understand your prolapse diagnosis:
- The severity of your prolapse
- What a mild, moderate or severe prolapse diagnosis means
- How your doctor measures your prolapse
- What your stage of prolapse means
- What a first, second or third degree uterine prolapse means
- Can your prolapse be repaired with exercises
Prolapse Exercises e-Book
International best selling prolapse exercise guide for women with prolapse and after prolapse surgery.
Prolapse Exercises teaches you how to:
- Exercise safely after prolapse surgery
- Reduce your risk or repeat prolapse
- Avoid unsafe exercises
- Choose pelvic floor safe exercises
- Reduce your risk of prolapse worsening
- Improve prolapse support
- Increase your strength and fitness
- Strengthen your core
- Lose weight
How Severe is Your Prolapse?
Your prolapse symptoms may feel awful but this doesn’t necessarily mean your prolapse is severe! Typical prolapse symptoms such as pelvic heaviness or lower back pain don’t correspond with prolapse severity.1
Some women are quite surprised to learn they have a prolapse during their regular pap smear. Others report quite bothersome symptoms with relatively minor prolapse severity.
Some prolapse symptoms tend to worsen in women with more severe prolapse. Vaginal bulging and being able to see your prolapse at the entrance of your vagina are prolapse symptoms that often worsen with more advanced prolapse. In other words you may or may not necessarily experience some of the established troublesome bowel, bladder or prolapse symptoms with different degrees of prolapse severity.
There is however a trend for some specific and bothersome prolapse symptoms to worsen in women with more advanced or severe prolapse.
What is a Mild, Moderate or Severe Prolapse?
Your doctor may have given you a prolapse diagnosis of mild, moderate or severe prolapse.
This is a very simple and general diagnosis of prolapse severity usually based on how troublesome your prolapse symptoms are and the amount of downward movement of your prolapse within your vagina evident during your examination. A big problem with this type of general assessment is that it’s not scientifically accurate or exact.
An accurate prolapse diagnosis must fully reproduce the full extent of the downward movement of your prolapse during your internal examination. This is why your doctor or physiotherapist will ask you to cough and strain downwards during your examination.
Most women need to be examined standing upright to fully reproduce the full extent of prolapse and provide them with an accurate prolapse diagnosis.
What Does Your Stage of Prolapse (POP-Q) Mean?
The POP-Q3 or Pelvic Organ Quantification is the internationally recommended prolapse classification system that was introduced to improve the accuracy of measuring prolapse severity. This system allows your health practitioner to provide a more accurate prolapse diagnosis than a general assessment.
If your gynaecologist uses POP-Q he or she will measure how far your prolapse moves downward within and/or out of your vagina by looking at the leading edge or the lowest part of your prolapse and measuring how far this moves downwards with coughing and bearing down or straining. Using this system your gynaecologist may have told you that your prolapse is somewhere on the range of Stage 0 to 4.
Understanding your POP-Q prolapse severity diagnosis
If your gynaecologist has used POP-Q to measure, he or she will classify your prolapse as follows:
Stage 0 – no prolapse is demonstrated during your examination
Stage 1 – the lowest part of your prolapse is more than 1 cm above your *hymenal ring
Stage 2 – the lowest part of your prolapse is within 1 cm either side of your hymenal ring
Stage 3 – the lowest part of the prolapse is more than 1 cm below the hymen but the vagina has not completely prolapsed
Stage 4 – the vagina is completely prolapsed outwards.
*Where is the hymenal ring?
Prolapse severity is measured using the hymenal ring as a fixed reference point in POP-Q assessment. The hymenal ring sits approximately 1cm within the external entrance or opening to the vagina. When the hymen (thin tissue across the entrance to the vagina) is broken by penetrative intercourse or using tampons the hymenal ring is the level where the hymen was previously positioned.
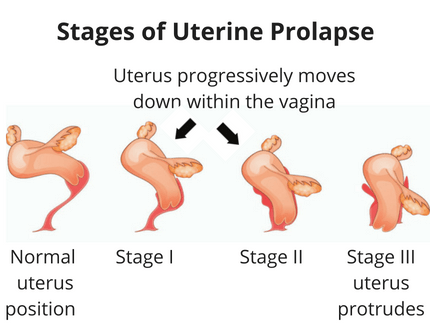
What is First, Second or Third Degree Uterine Prolapse?
Some gynaecologists still diagnose a uterine prolapse as first, second or third degree in severity.
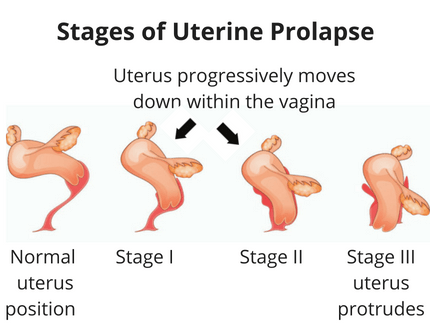
This system was used in the past to grade uterine prolapse by assessing how far the cervix had moved downwards in the vagina. The cervix is the muscular ring (feels like a nose tip) that sits at the very top of your vagina at the entrance of your uterus.
Understanding your Uterine Prolapse Diagnosis
- First degree uterine prolapse – the cervix moves down inside the vagina
- Second degree uterine prolapse – the cervix moves though the opening of the vagina with straining
- Third degree uterine prolapse – the uterus moves out of the vagina
Can Your Prolapse be Fixed With Pelvic Floor Exercises?
Recent research2 has shown that some women with mild to moderate prolapse (i.e. Stages 1- 2 as measured by POP-Q method), supervised pelvic floor muscle training including home pelvic floor exercises decreased prolapse severity and reduced specific prolapse symptoms.
This means that for women with mild to moderate prolapse (i.e. prolapse above the hymen) it may be possible to reduce prolapse symptoms and even avoid prolapse surgery with pelvic floor muscle training.
A lack of research means that it is currently unknown whether women with more severe prolapse diagnosis can reverse prolapse symptoms and severity with exercises.
Some women with more advanced or severe prolapse will require prolapse surgery or long-term support pessary management. The most appropriate time for you to proceed with prolapse surgery is a matter for you and your gynaecologist to discuss and determine based upon your prolapse diagnosis and other relevant factors.
Key Points About Prolapse Diagnosis
Understanding your prolapse diagnosis helps you make better informed decision about your future prolapse management.
The evidence suggests that for women with mild to moderate (Stage 1- 2) prolapse diagnosis, pelvic floor muscle training may be an effective method of reversing prolapse and reducing prolapse symptoms. If you can alleviate your prolapse symptoms, you may even feel less likely to need prolapse surgery!
ABOUT THE AUTHOR, Michelle Kenway
Michelle Kenway is an Australian Pelvic Floor Physiotherapist. Michelle lectures to health professionals and promotes community health through her writing, radio segments, online exercise videos and community presentations. She holds dual post graduate physiotherapy qualifications in women’s health and exercise.
References
1. Barber MD, Walters MD and Bump R (2003) Association of the magnitude of pelvic organ prolapse and presence of severity of symptoms (abstract #3 103). In International Continence Society, Florence.
2. Brækken, I. H., Majida, M., Engh, M. E., & Bø, K. (2010). Can pelvic floor muscle training reverse pelvic organ prolapse and reduce prolapse symptoms? An assessor-blinded, randomized, controlled trial. American journal of obstetrics and gynecology, 203(2), 170-e1.
3. Bump R Mattiason A Bo K, Brubaker L DeLancey J Klarskov P Shull B Smith A (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. American Journal of Obstetrics & Gynecology, 175:13.