Prolapsed bladder management involves identifying factors contributing to your prolapse and bladder support exercises to improve prolapse support. 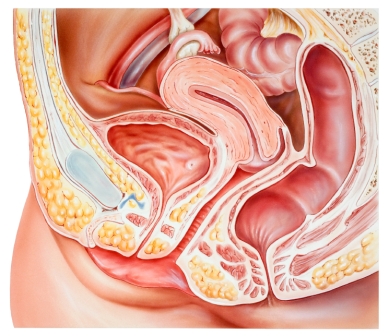
This Pelvic Floor Physiotherapist information helps you understand how to best manage your bladder prolapse, exercise safely and prevent recurrent bladder prolapse after bladder prolapse surgery.
Read on for Physiotherapist tips and techniques for prolapsed bladder management:
1. What is a prolapsed bladder?
2. What are the symptoms of a prolapsed bladder?
3. Does a bladder prolapse cause bladder leakage ?
4. What causes a bladder prolapse?
5. Tips for protecting by your bladder prolapse and after prolapse surgery
6. How to exercise safely with a bladder prolapse, exercises to avoid and those to choose
Prolapse Exercises e-Book
International best selling prolapse exercise guide for women with prolapse and after prolapse surgery.
Prolapse Exercises teaches you how to:
- Exercise safely after prolapse surgery
- Reduce your risk or repeat prolapse
- Avoid unsafe exercises
- Choose pelvic floor safe exercises
- Reduce your risk of prolapse worsening
- Improve prolapse support
- Increase your strength and fitness
- Strengthen your core
- Lose weight
1. What is a Prolapsed Bladder?
Bladder prolapse is commonly referred to as “dropped bladder” or “fallen bladder”, and is one type of pelvic organ prolapse. Bladder prolapse is relatively common in women and the risk increases with increasing age.
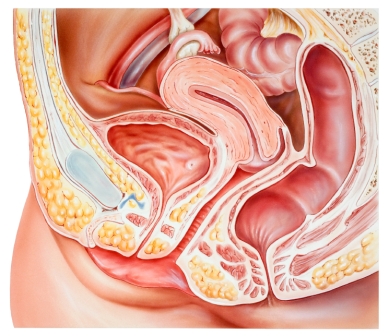
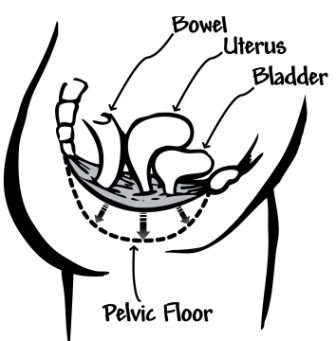
A prolapsed bladder occurs when when the bladder moves into the front wall of the vagina. Sometimes the front wall of the vagina is pushed down and out of the vagina and appears as a bulge at the entrance of the vagina. This occurs when there is a weakness in the pelvic floor support structures allowing the bladder to fall through the area of weakness. Bladder support structures include pelvic floor muscles and thick supporting tissues.
You can see the importance of maintaining a strong pelvic floor muscles with kegels after prolapse surgery from this diagram, especially if you have been diagnosed with a bladder 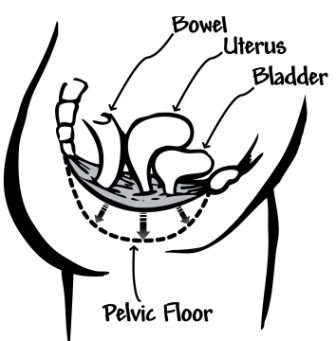 prolapse or after bladder prolapse repair surgery. Pressure from within the abdomen can push the pelvic floor (and bladder prolapse) downwards. Strong supportive pelvic floor muscles help to resist the downward pressure on your pelvic floor from everyday activities and exercise.
prolapse or after bladder prolapse repair surgery. Pressure from within the abdomen can push the pelvic floor (and bladder prolapse) downwards. Strong supportive pelvic floor muscles help to resist the downward pressure on your pelvic floor from everyday activities and exercise.
2. What are the Symptoms of Bladder Prolapse?
Bladder prolapse may present with a number of different prolapse symptoms. When the prolapse is very mild it may not produce any symptoms. Prolapsed bladder symptoms tend to become more apparent as the prolapse worsens. Some women report one or more of the following symptoms:
- Bulging, heavy sensation in the vagina, often worse at the end of the day
- Lump coming down inside and/or out of the vagina
- Difficulty inserting tampons
- Difficulty emptying the bladder with slow stream and sometimes incomplete bladder emptying.
3. Does Prolapsed Bladder Cause Bladder Leakage?
No, bladder leakage does not occur because of a bladder prolapse. Some women may suffer from a leaking bladder in addition to their prolapse.
Sometimes a bladder prolapse causes a small kink or bend in the urine tube (urethra) which actually decreases leakage during activities stressful activities for the pelvic floor such as coughing or sneezing and this is called occult stress incontinence (because it is usually hidden). This is the reason why women who are found to have stress incontinence and bladder prolapse by their specialist may have a bladder sling or procedure to reduce leakage at the same time as their bladder prolapse surgery. If the prolapse is surgically repaired and the woman also has underlying stress incontinence which she may not have know about then she may start to leak when the prolapse is repaired and the urine tube is straightened out.
4. What Causes Prolapsed Bladder?
There are many different factors that can cause or contribute to a bladder prolapse.
Common causes of a prolapsed bladder include:
- Pregnancy and childbirth (sometimes injury to the pelvic floor doesn’t appear until years later)

- Hormonal changes with menopause
- Ageing
- Constipation and straining repeatedly to empty the bowel.
Other factors which may contribute to bladder prolapse are:
- Being overweight
- Chronic coughing associated with smoking or asthma
- Heavy exercise including intense core training and heavy resistance training
- Previous pelvic surgery including surgery for urinary incontinence, sacrospinous fixation and perhaps hysterectomy.
5. Tips for Bladder Prolapse and After Bladder Prolapse Repair Surgery
Avoid:
- Constipation and repeated straining to use your bowels (see our free training video now on how to overcome bowel movement problems to learn how to empty and avoid straining)
- Heavy lifting, pushing/pulling, bending
- Smoking (to reduce coughing)
- High impact exercise (e.g. jogging, sit-ups, horse-riding, high impact aerobics)
- Heavy resistance exercises and intense core abdominal exercises
- Excessive weight gain
Do:
- Regular pelvic floor exercises or kegels after prolapse surgery – start after bladder prolapse surgery when you have your specialist’s approval to commence. If you are not sure seek further information on how to exercise your pelvic floor muscles (see our free training video on how to find and feel your pelvic floor muscles to the right of your screen, read Inside Out or check with your women’s health physiotherapist).
- Consider a pessary ring – pessary rings are designed to support the prolapse and minimise symptoms by sitting high inside the vagina. Women often find that using a pessary ring helps them to better exercise their pelvic floor muscles by lifting their prolapse and reducing dragging. Speak with your specialist about the feasibility of a pessary for your condition.
- Wear quality support underwear (briefs) or a pelvic when you are active
- Practice good bowel habits – choose bowel friendly foods and never strain to use your bowels. Some women find they can support their dropped bladder by holding a pad of toilet paper over the vagina when using their bowels.
- Alternate activities – avoid prolonged standing especially when recovering from pelvic floor repair surgery.
- Split tasks – do household chores over a few days rather than all in one day.
- Lose weight if you are overweight.
- Rest in the afternoon and elevate your legs if possible.
- Manage chronic cough, chronic hay fever and sneezing by visiting your doctor
- Practice good posture – to promote good pelvic floor function
- Choose low impact exercise
6. Safe Exercise With Prolapsed Bladder?
Many everyday exercises can increase pressure on your pelvic floor and worsen your bladder prolapse symptoms or even contribute to repeat prolapse after already having had prolapse surgery. You need to make sure that you are fully informed about the exercises that are suitable for you if you are living with a prolapse.
1. Fitness exercises that reduce pressure on the pelvic floor
Fitness exercise should be low impact to reduce pressure on the pelvic floor. This means choosing exercises keeping one foot at least on the ground with exercise. This is quite different to high impact exercise such as running or jumping where both feet are off the ground. Low impact exercises include:
- Cycling
- Walking
- Dancing
- Bush walking
- Swimming
2. Strength training and abdominal exercises
Many everyday strength training and abdominal exercises have the potential to increase the downward pressure on the pelvic floor. These are some exercises to avoid with a bladder prolapse:
- Intense abdominal strength exercises and abdominal exercise machines which have the effect of increasing pressure on the pelvic floor
- Specific strength exercises such as leg press and wide leg squats that increase pressure on the pelvic floor and prolapse
- Heavy lifting and straining when lifting weights
- Breath holding when lifting weights-breathe out with the effort of lifting, pushing or pulling
- Plus sit on a ball or a bench for all your strength exercises wherever possible to support your pelvic floor
For further information articles and free videos on safe exercise with a prolapsed bladder and after prolapse surgery include prolapse protection for strength training and 12 abdominal exercises to avoid with prolapse or after prolapse surgery.


 prolapse or after bladder prolapse repair surgery. Pressure from within the abdomen can push the pelvic floor (and bladder prolapse) downwards. Strong supportive pelvic floor muscles help to resist the downward pressure on your pelvic floor from everyday activities and exercise.
prolapse or after bladder prolapse repair surgery. Pressure from within the abdomen can push the pelvic floor (and bladder prolapse) downwards. Strong supportive pelvic floor muscles help to resist the downward pressure on your pelvic floor from everyday activities and exercise.


